A 9-year-old female neutered Old English Sheepdog was presented to SCVS as an emergency, having suffered three episodes of collapse prior to referral. The dog was reported to have recovered uneventfully from the first episode which occurred two weeks prior to referral. Over the previous month, the owner reported that the dog had been intermittently restless and episodes of suspected abdominal discomfort were observed. A single episode of vomiting was reported and the dog was seen to adopt a ‘praying posture’ on multiple occasions. The dog was presented to the referring vet having suffered two episodes of collapse within an eight hour period. Investigations showed a PCV of 21% and as such referral for further investigation and treatment was sought.
At the time of presentation, the dog was quiet but alert and responsive. Physical examination showed pale mucous membranes and mild tachycardia (HR-128). Abdominal palpation was hindered slightly by the nervous disposition of the patient but there was a suspicion of discomfort and splenomegaly. Systolic blood pressure was measured at 145mmHg and all other vital parameters were within normal limits.
Initial complete blood count showed the following abnormalities. The remainder of the CBC, biochemistry and urinalysis was unremarkable and prothrombin and activated-partial thromboplastin times were normal.
| RBC |
* 2.82 x10^12/L |
Low (5.0-8.5) |
| Hb |
7.1 g/dl |
(12.0-18.0) |
| HCT |
* 21.1 % |
Low (37.0-55.0) |
| MCV |
74.8 fl |
(60.0-80.0) |
| MCH |
25.2 pg |
(19.0-26.0) |
| MCHC |
33.6 g/dl |
(30.8-37.0) |
| RDW |
13.4 % |
(12.9-17.8) |
| Platelets |
* 30 x10^9/L |
Low (160-500) |
| Reticulocyte % |
0.5 % |
|
| Reticulocyte count |
14.10 x10^9/L |
|
The major abnormalities detected were non-regenerative anaemia (reticulocyte percentage <1% and absolute reticulocyte count <60×10^9/L) and severe thrombocytopenia (blood film examination estimated platelet count to be 50-70×10^9/L). Given the apparent acute onset of this episode, it was thought the anaemia was likely pre-regenerative (it can take up to 5 days for the maximal bone marrow response to be seen). Anaemia can be caused by three major mechanisms; haemolysis, blood loss (internal or external haemorrhage) or decreased red cell production. Haemolysis was considered to be the most likely mechanism in this case. Decreased production due to a primary bone marrow disease was considered less likely given that the neutrophil count was normal but was still considered possible. Internal and external haemorrhage were considered unlikely given that the patient was normotensive and total protein concentrations were within normal limits.
General differential diagnoses for haemolytic anaemia include:
- Immune-mediated haemolytic anaemia (primary or secondary to neoplasia, infectious agents, drugs/toxins or systemic inflammatory disease such as SLE)
- Infectious agents causing direct haemolysis such as Babesia spp (Babesiosis has been reported in UK dogs with no history of travel)
- Inherited red cell defects such as phosphofructokinase (PFK) deficiency in the Springer Spaniel and pyruvate kinase (PK) deficiency in the West Highland White Terrier
- Oxidative red cell damage due to ingestion of toxins such as zinc, onions, garlic methylene blue etc.
- Severe hypophosphatemia (typically associated with severe metabolic derangements such as diabetic ketoacidosis or refeeding syndrome)
- Microangiopathic anaemia associated with splenic pathology, dirofilariasis etc.
General differential diagnoses for thrombocytopenia include:
- Immune-mediated thrombocytopenia (primary or secondary to neoplasia, infectious agents, drugs/toxins or systemic inflammatory disease such as SLE)
- Decreased platelet production associated with bone marrow disease such as myelodysplasia, myelofibrosis or myelophthisis
- Platelet loss associated with haemorrhage (typically does not result in severe thrombocytopenia)
- Platelet consumption associated with DIC (can potentially result in moderate-marked thrombocytopenia)
- Platelet sequestration (can occur with diseases causing splenomegaly or within the pulmonary vasculature in septic patients but typically is not associated with severe thrombocytopenia)
At this point it was thought that the most likely differential diagnosis was immune-mediated haemolytic anaemia and thrombocytopenia, also known as Evan’s syndrome (OESD are one of the breeds considered predisposed to IMHA and IMTP). A primary aetiology was considered possible but given the suspicion of splenomegaly on abdominal palpation, there was concern that an underlying disease, particularly neoplasia, may be present. The patient was considered stable and as such no specific treatment was instigated while awaiting the results of further diagnostics. Slide-agglutination and Coomb’s tests were requested at the lab and diagnostic imaging was performed to investigate the possibility of an underlying cause.
Radiographs of the thoracic cavity were unremarkable but abdominal radiographs confirmed marked splenomegaly (see picture below). An abdominal ultrasound was performed and confirmed marked generalised splenomegaly and associated mass effect with the small intestines displaced caudally and gastric axis displaced cranially. The borders of the spleen were considered smooth with no changes suggestive of a mass lesion were seen. Normal flow with the splenic vasculature was documented. The remainder of the abdominal viscera were considered normal and there was no abdominal free fluid.
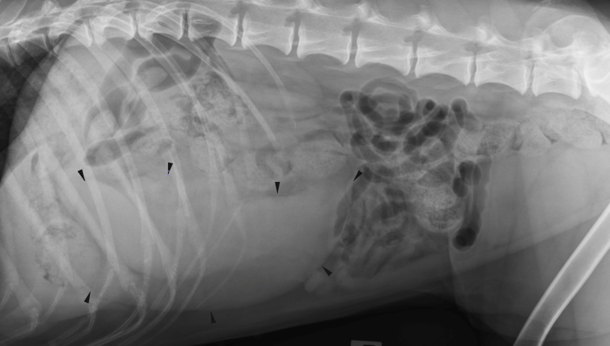
Arrows highlight the enlarged spleen with associated caudal displacement of the small intestines
Differential diagnoses for generalised splenomegaly include:
- Round cell neoplasia such as lymphoma, histiocytic sarcoma, mastocytosis
- Splenic congestion due to pre, intra or post hepatic portal hypertension
- Splenic torsion
- Splenitis (potentially due to vector-borne disease, tuberculosis, leptospirosis)
- Massive extramedullary haematopoiesis or extravascular haemolysis associated with immune-mediated haemolysis
It was assumed that an underlying primary splenic pathology such as round cell neoplasia was contributing to the clinical and clinicopathological changes seen and as such, ultrasound-guided aspirates of the spleen were taken and submitted for cytology. A moderate amount of haemorrhage occurred following aspiration of the spleen and as such, serial PCV/TS measurements were taken overnight. Despite ongoing intra-abdominal haemorrhage, the dog appeared to improve clinically and the each consecutive measurement showed an increasing PCV. The following morning, the dog appeared stable with all vital parameters within normal limits and repeat CBC returned the following results:
| RBC |
* 4.93 x10^12/L |
Low (5.0-8.5) |
| Hb |
12.2 g/dl |
(12.0-18.0) |
| HCT |
* 35.9 % |
Low (37.0-55.0) |
| MCV |
72.8 fl |
(60.0-80.0) |
| MCH |
24.7 pg |
(19.0-26.0) |
| MCHC |
34.0 g/dl |
(30.8-37.0) |
| RDW |
14.3 % |
(12.9-17.8) |
| Platelets |
* 61 x10^9/L |
Low (160-500) |
| Reticulocyte % |
2.7 % |
|
| Reticulocyte count |
133.11 x10^9/L |
|
The RBC had almost returned to normal but there was still marked thrombocytopenia. Slide agglutination and Coomb’s tests returned negative results and this in combination with the dramatic increase in RBC over the space of 24 hours and without any specific treatment made a haemolytic process extremely unlikely. Serologies for Erhlichia, Anaplasma, Borellia and Bartonella spp and PCR for Babesia spp all returned negative results. Cytology of the splenic aspirated returned results consistent with normal splenic tissue. The exact underlying pathology remained elusive but we hypothesised that the marked splenomegaly had led to sequestration of both red cells and platelets and upon aspiration of the spleen, there was marked release of red blood cells back to the circulation and this led to the resultant increase in red blood cell count. The cause of the splenomegaly remained unknown. A search of the human literature was performed and a disease known as Primary or Idiopathic Hypersplenism was identified. Affected people can suffer from a combination of cytopenias (including anaemia, thrombocytopenia and neutropenia) and have concurrent marked splenomegaly. The treatment in affected people is splenectomy and this typically leads to a rapid and complete resolution of clinical and clinicopathological signs. The condition has also been documented in ferrets but has not yet been reported in dogs or cats.
The possibility of Primary Hypersplenism was considered in this case, however an underlying neoplastic process was still considered possible. It was decided that the most appropriate next diagnostic and therapeutic step would be to remove the spleen. Given that the dog remained stable without any specific treatment thus far, she was discharged for three days in the hope that the platelet count would increase prior to surgery. When readmitted in advance of surgery, both the RBC and platelet count were within normal limits. Repeat abdominal imaging confirmed persistent splenomegaly. The dog was transferred to the soft-tissue surgery department and splenectomy was performed with the entire spleen then submitted for histopathological analysis. The dog recovered well from surgery and was discharged the following day.
Histopathology of the spleen showed expansion of the red pulp with arteriolar congestion and sinusoidal proliferation, changes consistent with chronic congestion. There was peripheral fibrous stromal proliferation and reorganisation and no overtly atypical / neoplastic cells were seen. These changes are similar to those seen in sections of spleen taken from affected people.
The dog in this case has been diagnosed with Primary Hypersplenism and to our knowledge, this has not been previously described in dogs. The mechanism for both the anaemia and thrombocytopenia is assumed to be due to splenic sequestration. As mentioned above, sequestration of platelets is a recognised mechanism for mild-moderate thrombocytopenia in dogs but sequestration has not been previously documented as cause of anaemia in dogs. The exact aetiology in affected humans remains unknown but hypotheses have included splenomegaly secondary to cirrhotic liver disease and associated portal hypertension or occult splenic lymphoma. Portal hypertension has been documented in a number of affected people. Portal pressures were measured intra-operatively in our case and found to be normal.
Subsequent recheck examinations and repeat haematology and biochemistry have not detected any abnormalities and the CBC has remained within normal limits. The dog’s owners report that she has returned to her bouncy, playful self and they feel that she is happier than she has been in months. This was a very interesting case and we hope that the dog continues to do well. We are very interested in following her progress long-term.
Click here for more information on our internal medicine department.