Jenny, a 10-year-old crossbreed, was presented to her referring vet with a history of reduced appetite and weight loss for a few weeks. The vet had found her total calcium to be high on several occasions and her urine specific gravity to be consistently low (1.015 & 1.005).
After performing an ACTH stimulation test, obtaining thoracic and abdominal radiographs, which were unremarkable, Jenny’s vet organised referral to SCVS for further investigations.
Differentials to consider in hypercalcaemic animals follow the mnemonic HARD IONS. Hyperparathyroidism, Addison’s, Renal disease, vitamin D overdose, Idiopathic (cat only), Osteolytic disorders, Neoplasia (Lymphoma, anal sac adenocarcinoma, multiple myeloma), Spurious.
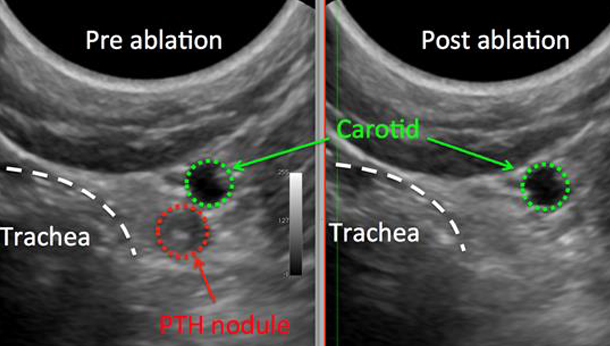
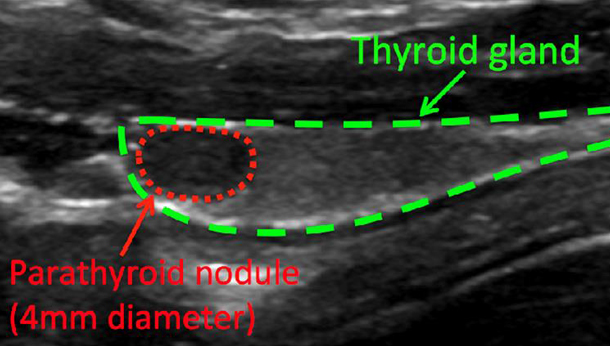
Physical examination was unremarkable. Ionised calcium was 2.28 mmol/L [1.12-1.4] and Jenny was moderately azotaemic (urea 16.3 mmol/L, creatinine 216 mol/L). Abdominal ultrasonography failed to reveal any abnormalities. Parathyroid ultrasonography revealed a left-sided parathyroid nodule. Jenny immediately underwent percutaneous ultrasound-guided ethanol ablation of the nodule. It took fewer than 24 hours from initial presentation to SCVS for normalisation of Jenny’s calcaemia.
Jenny’s owner was warned that signs of hypocalcaemia could occur within 1-7 days of treatment owing to transient atrophy of the contralateral parathyroid gland. Jenny’s calcium level was monitored and as is often the case when the initial calcium level is very high she developed hypocalcaemia 2 days post-ablation. Supplementation with oral calcitriol and calcium gluconate was started. It took a week for the ionised calcium to reach the target level of 0.9 mmol/L and we expect to be able to slowly discontinue supplementation over the next 3-4 months.
Key Points
- Hypercalcaemia detected on total calcium measurement should always be followed up and confirmed by measuring ionised calcium as most causes of hypercalcaemia are sinister and persisting hypercalcaemia can lead to permanent renal injury.
- Primary hyperparathyroidism is less common than malignancy-related hypercalcaemia but carries a good prognosis if detected and treated early. Clinical signs may have been overlooked by the owners but can include muscle weakness and lethargy, polyuria and polydipsia (PU/PD), lower urinary tract signs, anorexia, weight loss, constipation and vomiting.
- Older dogs (mean age 10.5 years) are affected by this condition with an over-representation in the Keeshond. Many have concurrent urolithiasis (calcium oxalate) from increased calciuresis, which is one reason why abdominal ultrasonography should always be performed in these dogs.
Definitive Diagnosis
In addition to hypercalcemia (total and ionised), low to normal phosphate, high to normal PTH and low PTHrp and low USG. Cervical ultrasonography often shows a singular (likely adenoma) or multiple (likely hyperplasia) enlarged parathyroid gland/s. Azotaemia is seen in longstanding cases.
Treatment
For a solitary adenoma, surgical parathyroidectomy is usually curative. Alternatives to surgery are percutaneous ethanol injection (PEI) or heat ablation, which have a high success rate as well. Surgical removal of 3 of 4 affected glands when all are affected by hyperplasia will result in eucalcaemia but the disease will likely reoccur, typically within months to one year.
PEI or Heat Ablation for the Treatment of Primary Hyperparathyroidism
Ultrasound guided PEI or heat ablation can be utilised safely for the treatment of primary hyperparathyroidism in dogs in the referral setting with a success rate of approximately 90%.
- Side effects from this procedure are minimal and transient.
- More than one injection may be necessary for successful therapy.
- After a successful injection total calcium, ionized calcium and PTH concentration normalise within 2-5 days.
- Multiple parathyroid masses can be injected sequentially.
- Surgical excision is possible after unsuccessful PEI or heat ablation therapy.
- Specialised ultrasonographic equipment and expertise are necessary.
Post-treatment Monitoring
Intensive post-treatment monitoring (ideally hospitalisation for 5-10 days with twice daily calcium monitoring) for hypocalcaemia is necessary after surgery, PEI or heat ablation. Calcium and vitamin D need to be supplemented in some cases when clinical or profound hypocalcaemia occur. Supplementation may be worthwhile prophylactically in cases where the pre-treatment calcium is very high (> 3.5mmol/L).