Otitis externa, inflammation of the external ear canal, with or without middle ear involvement, is very common in dogs and quite common in cats. Many different factors can cause or exacerbate otitis and recognition and correction of these is the key to successful management. Scrupulous note of the historical features, thorough examination of the ear and collection of appropriate samples constitute the minimum database. Selected cases may need further investigations, including imaging of the middle ear.
History
It is important obtain a complete history in patients with either acute or chronic otitis externa. Relevant considerations include:
- Owner’s complaint - often head-shaking, ear rubbing and/or discharging and malodour
- Signalment – several breeds, due to the conformation of the pinnae and ear canals and due to their susceptibility to other diseases, are predisposed to develop otitis; young dogs are predisposed to otodectic mange and elderly dogs to endocrinopathies
- Lifestyle – outdoor activities such as walks in fields may predispose to foreign body and frequent swimming to moisture of the are canals
- Acute onset with frenzied head-shaking may again indicate foreign body
- Chronic cases with skin disease elsewhere suggests otitis is part of a more generalised skin disease
- Seasonal recurrence suggests atopic disease
- Unsuccessful previous treatments may indicate presence of resistant organisms or onset of drug eruptions to topical medications
Physical Examination
Full general and dermatological examination is paramount. This enables to identify underlying primary causes of the otitis and eventual neurological signs of otitis media and otitis interna.
The clinical findings vary with the cause:
- Tumours, parasites and foreign bodies may be evident upon otoscopy

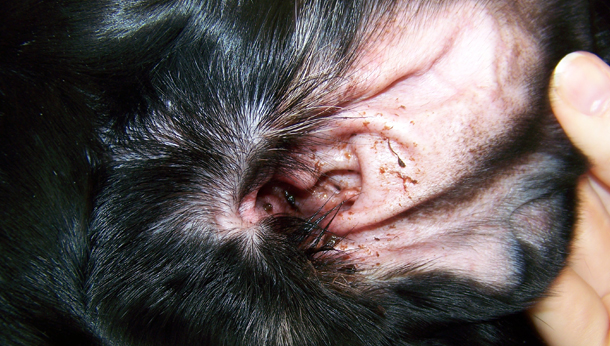
- Erythema of the medial pinna and vertical canal suggests an allergic aetiology (Fig. 1)
- Dry, brown, granular discharge is seen with Otodectes infestation
- Moist brown discharge can be seen with staphylococcal and Malassezia infections (Fig. 2)
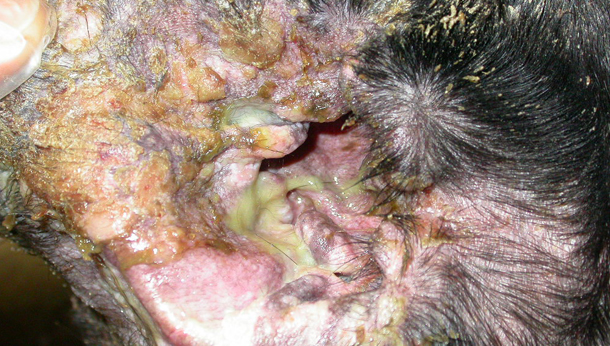
- Purulent, greenish, foul odour exudate indicates gram negative bacterial infection (Fig. 3)
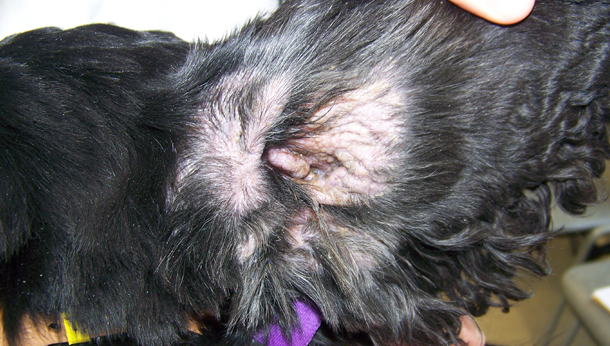
- Chronic cases may have thickened, pigmented skin (Fig. 4) and para-aural abscesses
- Cornification disorders may have changes in coat quality, colour and density or scale formation
- Facial nerve paralysis and Horner’s syndrome may are indicative of otitis media

- Head tilt, circling, falling toward the affected side, horizontal nystagmus and asymmetric ataxia are indicative of otitis interna (Fig. 5)
- Some cases of otitis media/interna may also show loss of hearing
- External palpation of the ear canals may reveal pain, thickening and hard consistency, with latter indicative of mineralisation of the cartilages
Otoscopy
Otoscopy is visualisation of the ear canal with an otoscope. Otoscopes available in veterinary medicine include:
- Closed - Good view; limited access; can perform tympanometry
- Open or surgical - Slight inferior view; excellent access; best choice if you are limited to one otoscope
- Video otoscope - Excellent view and access; can record images
Careful visualisation will identify foreign bodies, Otodectes, inflammatory changes, ulceration, stenosis, condition of the tympanic membrane (tough in many cases otoscopy alone is often not sufficient for detecting all changes in the tympanic membrane and otitis media), amount and type of exudate as well as the degree and type of chronic changes. The normal ear canal should have a thin, smooth and pale pink appearance. The most common pathological findings include:
- Swollen, moist erythematous lining of the ear canals suggestive of acute inflammation
- Firm, fibrous, indurated appearance suggestive of chronic changes
- Erythema confined to the vertical portion of the ear canal in absence of exudate, suggestive of allergic otitis (food induced or non-food induced atopic dermatitis)
- Erosions and ulcers accompanied by purulent exudate are seen when Gram negative bacteria complicate the otitis
- ‘Cobblestone’ appearance to the lining of the ear canals suggestive of sebaceous and ceruminous hyperplasia. In some dogs this may develop into moderate to large, single or multiple polyp-like growths
- Foreign bodies, tumours and parasites
In many cases complete otoscopic examination may be impaired by exudate, stenosis, and excess of hair. If otoscopy is prevented by these findings, is preferable not persist (especially in animals with painful ears). Such cases should be examined under sedation/anaesthesia and, in presence of stenosis, is preferable to review the animal after a 1 - 2 week (depending on the severity of the clinical signs) course of oral glucocorticoids.
Examination of the visible part of the tympanic membrane may reveal changes (thickening, bulging, loss of transparency, partial rupture) or complete absence.
The integrity of the tympanic membrane can also be assessed by tube palpation. This is done through the surgical otoscope head but is more valuable when done through the video otoscope. Debris can often mimic a tympanic membrane; a feeding tube or catheter will, however, pass through into the middle ear without resistance. In normal dogs and cats ear the tip of the tube can always be visualised; if the tube tip goes to a point where it cannot be seen that indicates pathology.
Another method to assess the tympanic membrane status is by tympanometry. Air is introduced into the ear canal via a closed otoscope. The tympanic membrane should flex back and forth; reduced movement or a bulging membrane suggests that there is fluid or debris in the middle ear. This is difficult technique to perform and assess, and it is not routinely done.
Microscopic Evaluation
The search of parasites (Otodectes cynotis, Demodex spp.) can be performed examined under low power (10x objective) the otic exudate admixed in mineral oil.
Cytology
Cytology is a quick and easy procedure; it is very useful to identify microbes, inflammatory or neoplastic cells and monitor the progress of treatment. Cytology should be performed from both ears in bilateral otitis and from ear canals and middle ear (when otitis media is present or suspected) as the findings may differ and influence your choice of treatment.
A swab is inserted into the horizontal ear canal to obtain sample of the otic exudate and then rolled onto a glass microscope slide and stained with a modified Wright’s stain. The specimen is then microscopically examined. It is essential to remember that cytology is most important in identifying micro-organisms, as the discharge does not always reflect the nature of the infection. Ear cytology is necessary at the initial examination and at each re-assessment. Microbial culture and sensitivity from the horizontal canal is not always required. It is performed in chronic recurrent or unresponsive cases, when otitis media is suspected and when rods are seen on cytology; in these cases Pseudomonas is suspected, which may be multi-drug resistant. Studies have shown that the organisms in the external ear canals and middle may be different and/or have different antibiotic sensitivity patterns. If possible, therefore, it is worth taking material for culture from both the external ear canal and middle ear.
Myringotomy
Latrogenic rupture of the tympanic membrane is indicated when otitis media is suspected to take samples for cytology and culture from the tympanic bulla. It should be performed under general anaesthesia and under direct visualization after lavage of the external ear, when the canal is dry. The preferred method used by the author is using a 6 F urinary catheter cut obliquely to a 60° and attached to a 2 ml syringe containing sterile saline solution. The catheter is advanced trough the ventral and posterior quadrant of the membrane with subsequent aspiration of the fluids. An aliquot can be used for direct cytological examination and the remaining for culture.
Diagnostic Imaging
Diagnostic imaging (radiography, CT, MRI) may be used to evaluate the ear, especially the middle ear for bony changes and other irreversible pathology that might indicate the need for surgery rather than medical therapy. Ear imaging is indicated in the following cases:
- Recurrent or severe otitis with suspected otitis media
- Para-aural swelling
- Fistulous tracts
- Trauma
- Inability to open the mouth
- Neurological dysfunctions
- Naso-pharyngeal polyp
- Complications following surgery
Techniques available include:
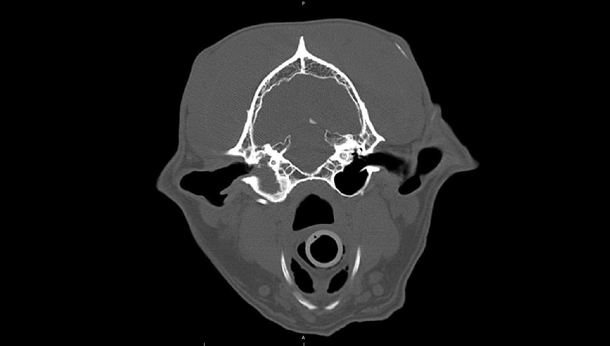
- CT – this technique provides excellent images of bony structures and it is also very sensitive and specific for stenosis and occlusion of the ear canals and soft-tissue filling of the middle ear (Fig. 6, courtesy of Livia Benigni). CT, if available, is quick and easy to perform and interpret. However, normal findings do not rule out otitis media.
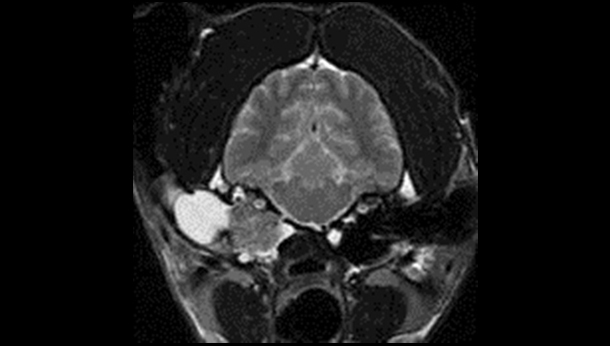
- MRI – it provides a better resolution of soft-tissue structures compared to CT or radiography. MRI is therefore better for imaging soft-tissue structures such as neoplasia (Fig. 7, courtesy of Ruth Dennis) in or around the ears, but it is less good for imaging and differentiating the cartilage of the ear canal and bony wall of the tympanic membrane. MRI takes longer to perform than CT and is more expensive.