Written by Andrew Craig, BVSc, PGCertSAS, DipECVS, MRCVS.
Daisy, a six-year-old female Maltese terrier crossbreed was referred to SCVS for management of a dorsal cranial mass. A biopsy had been taken by the referring vet which revealed findings consistent with a multi-lobular bone tumour. On initial presentation, Daisy was bright and alert. On examination, there was a hard mass, approximately 5cm in diameter on the midline involving part of the frontal and parietal bones.
Blood sampling was performed for haematology and serum biochemistry and revealed mild elevations in liver enzymes, otherwise there were no significant abnormalities. Under anaesthesia, computed tomography (CT) revealed a large “popcorn-like” mass of the dorsal aspect of the cranium affecting the frontal and temporal bones and mild associated frontal and temporal lobe compression.
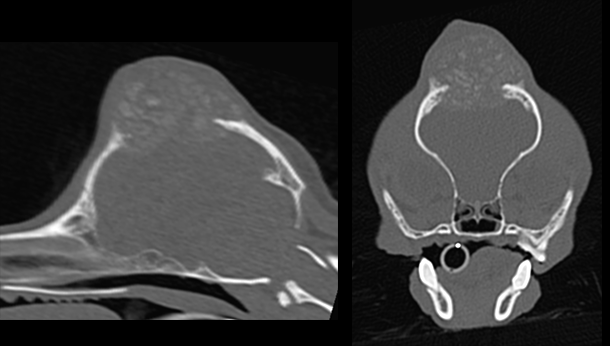
Above: Sagittal (left) and transverse (right) computed tomography images revealing a large popcorn-like mass of the dorsal aspect of the skull affecting the frontal and temporal bones
The “popcorn-like” appearance was typical of a multi-lobular tumour of bone (multilobular osteochondrosarcoma), consistent with the histopathological diagnosis. There was no evidence of metastatic disease on the remainder of the CT images. A multilobular bone tumour is an uncommon tumour attributable to abnormal cellular activity arising from the periosteum of bones formed by intramembranous ossification with the cells of origin periosteal cells of the common chondrocranium and viscerocranium, both of which share a common embryonic origin (VSSO website)
The options were discussed with the client including radiotherapy and surgical excision of the mass. Surgery is typically recommended, although there some anecdotal reports regarding the use of radiation in addition to a case report showing response to Samarium radiation in three dogs. There is no known effective chemotherapy for metastatic disease, however due to the slow growing nature of the tumour, survival times greater than 12 months have been reported with pulmonary metastasis (Dernell et al, 1998).
Daisy returned to SCVS several weeks later at which point it was clear that the tumour had grown considerably in that time frame. This type of tumour typically grows slowly, therefore the recent growth rate made us suspect that Daisy’s prognosis would have been guarded without surgery. The clients elected to proceed with surgery.
The SCVS Anaesthesia service was heavily involved in the anaesthetic due to the potential risks associated with a craniectomy. Under anaesthesia a CT was repeated to aid in surgical planning.
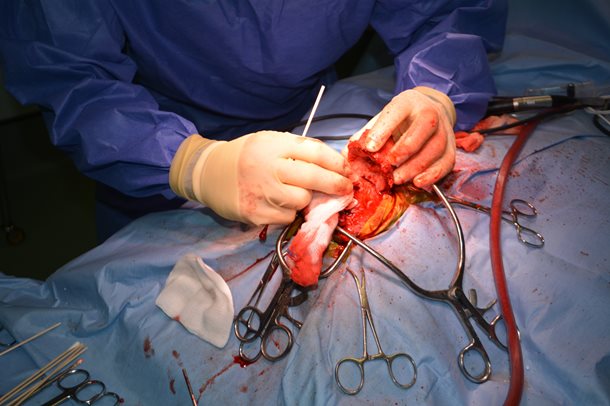
A dorsal approach to the tumour was performed permitting the previous biopsy tract to be excised with the tumour. A craniectomy was performed and the mass excised en bloc.
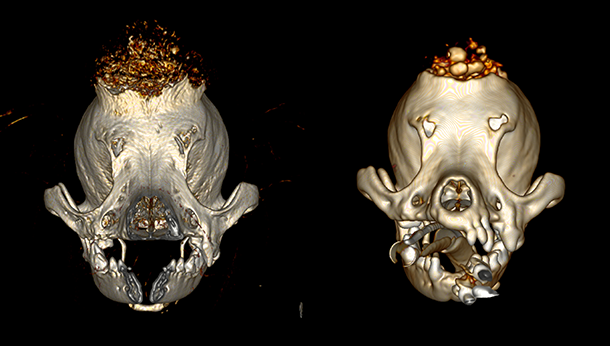
Above: CT images showing the increase in size of the lesion. The left image was acquired at initial presentation and the right was acquired pre-operatively.

Above: Daisy prepped for surgery, showing the size of the tumour.

Above: Intra-operative images revealing the cranium being burred. Below: and the tumour being removed (right) with lateral margins of 1-2cm of normal bone.
A titanium mesh was contoured and secured to the remaining parietal and frontal bones with eight self-drilling screws. Post-operative CT confirmed satisfactory implant-positioning.
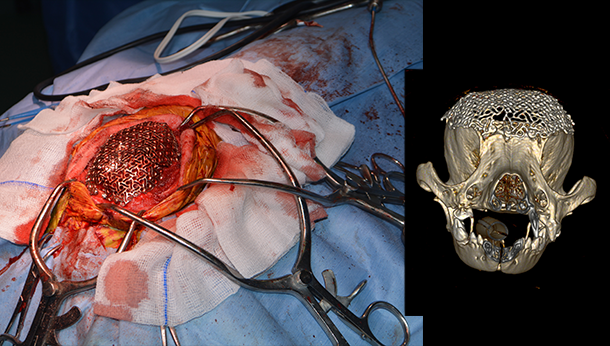
Above: intra-operative (left) and post-operative computed tomography image (right) revealing satisfactory implant positioning.
Daisy recovered uneventfully from anaesthesia and remained hospitalised for a few days for intravenous analgesia and close monitoring. No complications were encountered during hospitalisation and she was extremely bright and playful when discharged two days following surgery. Histological examination of the mass confirmed a multi lobular bone tumour of the cranium.
Client telephone and e-mail communications over the weeks following surgery reported Daisy had returned to normal. More recently (approximately six months following surgery) the client reported Daisy had suffered from a few minor seizures. The seizures have been completely controlled with anti-epileptic medications, therefore she continues to lead a normal life. Repeat imaging would be required to determine the cause of the seizures, however, as Daisy was doing clinically well on her medications we elected not to perform the investigations. Possible causes of the seizures include recurrence of the tumour or from inflammation of the meninges. If the cause of the seizures is attributable to recurrence of the tumour then this will have an impact on the long term prognosis.

Overall we are very pleased with her progress and to have given Daisy many more months with her owner.
References:
Darnell WS, Straw RC, Cooper MF, Powers BE, LaRue SM, Withrow SJ. Multi lobular osteochondrosarcoma in 39 dogs: 1979-1993. J Am Anim Hosp Assoc. 1998; 34: 11
VSSO (viewed April 2019) Cancer in dogs by tumour type. https://vsso.org/index.php/education-new/cancer-information-new/cancer-in-dogs-by-tumor-type-new?id=302:bone-mlo&catid=4