Written by Tony Ryan, MVB, CertSAS, DipECVS, MRCVS.
Many cases at SCVS require the input of multiple specialists, and we are very lucky to be able to call upon the expertise and experience of 21 Veterinary Specialists in eight disciplines, in addition to an experienced nursing team. One such case that recently benefited from our multi-disciplinary approach was George, a three month old Pug.
George was initially referred to the Neurology Service at SCVS, for investigation of acute onset forebrain signs, including dullness, head pressing and ataxia. Even though he was only three months old, George had been quite unlucky, and had lost his left ear, which was bitten off by his mother shortly after birth. He then developed a corneal ulcer affecting his right eye, which required a corneal graft procedure one week before referral.
On presentation, he was obtunded, circling to the left hand side, with head pressing and an absent menace bilaterally. These signs were consistent with a diffuse forebrain disease. Routine haematology and serum biochemistry revealed hyperammonaemia, elevated bile acids, mild elevations in hepatic parametres, panhypoproteinemia and anaemia.
Hepatic encephalopathy due to portosystemic shunt, or other congenital vascular liver disease was suspected and he was transferred to the Internal Medicine Service. Medical management with intravenous fluids and antibiotics, lactulose, initially via enemas, and then orally, was commenced. He recovered over the following 48 hours and CT angiography was performed by the Imaging Service which revealed the presence of a single extrahepatic PSS (gastro-caval).
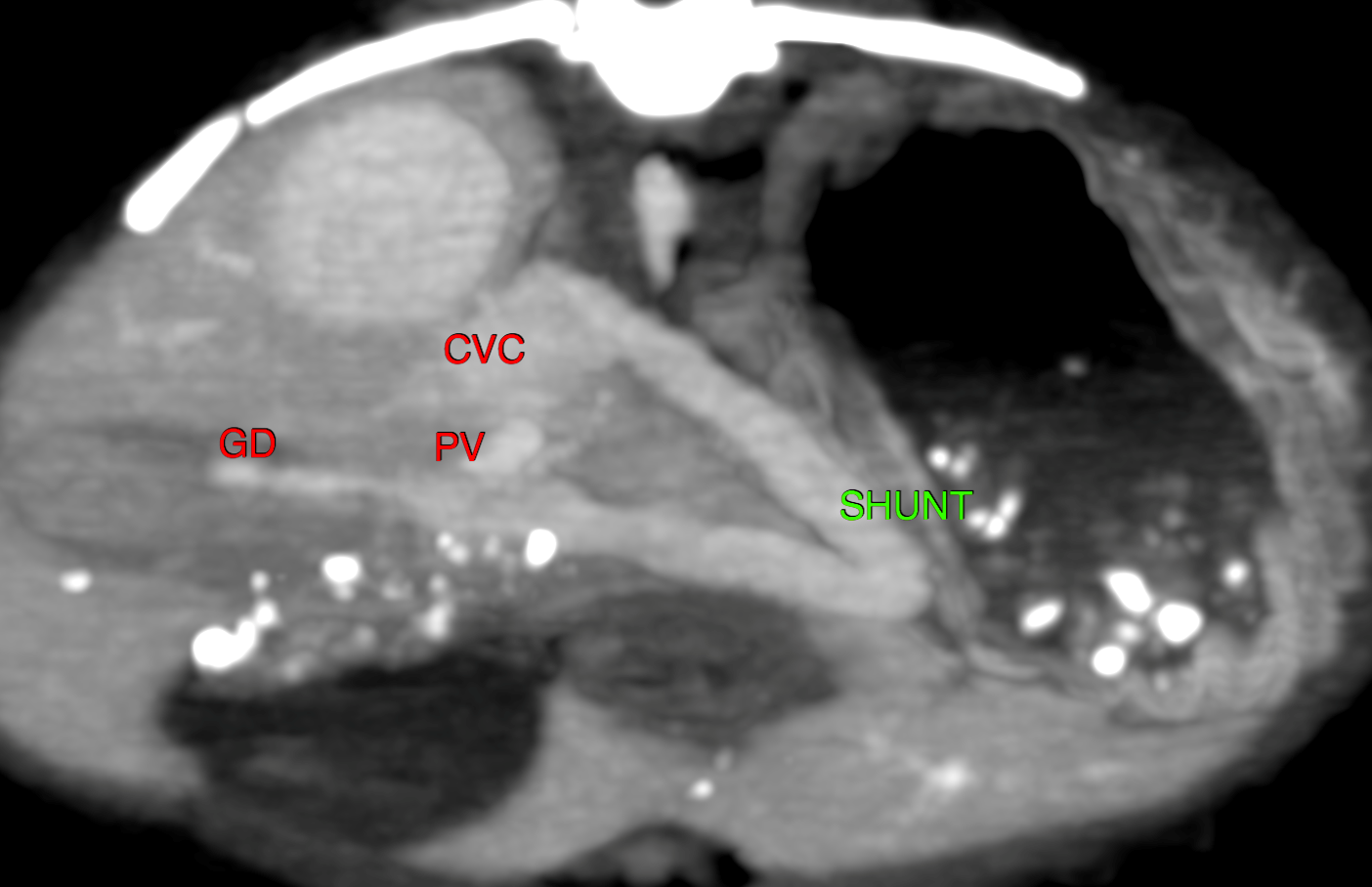
Figure 1. A large and tortuous vessel arising from the right gastric vein and entering the caudal vena cava just caudal the porta hepatis. (GD: gastroduodenal vein, PV: portal vein, CVC: caudal vena cava).
Three weeks later, George returned for reassessment with the Soft Tissue Service, and the owners reported a marked difference in his behaviour and demeanour following commencement of medical treatment. It was decided to proceed with surgical attenuation, and under the care of our Anaesthesia Team, a ventral midline coeliotomy was performed. An abnormal vessel was identified entering the caudal vena cava from the left hand side at the porta hepatitis, as described on CT. A 3.5mm ameroid constrictor was applied around the shunting vessel and a liver biopsy was taken.
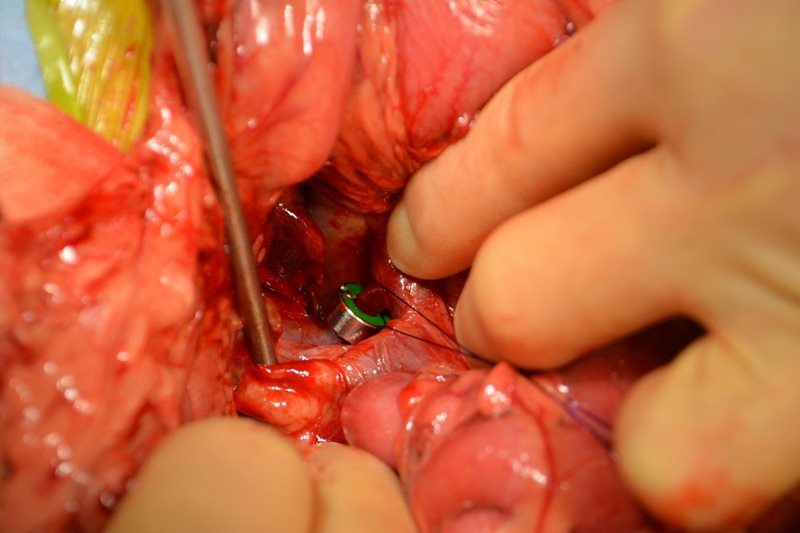
Figure 2. Ameroid constrictor applied around the portosystemic shunt at the level of the caval insertion.
George recovered uneventfully in ICU and was discharged a few days later to continue courses of metronidazole, amoxicillin and lactulose, as prescribed by the Internal Medicine Service. He returned one month following surgical attenuation. He had grown considerably, having gained 1.2kg, to weigh 3.2kg. The owners reported a marked improvement in his demeanour and appetite, and felt he was now a “normal” dog, similar to his sister.

Figure 3. George recovering from sugery
Routine haematology and serum biochemistry revealed a marked improvement in biochemical parametres, with his bile acids being within normal limits. Under sedation, ultrasound revealed normal hepatopetal portal vein flow, normal portal velocity with no continued shunting.
At SCVS, surgical attenuation of extrahepatic portosystemic shunts is the preferred treatment, and has been shown to result in improved survival and a lower frequency of ongoing clinical signs, when compared to medical management alone. Complete attenuation of the shunting vessel is desirable, but it may not be possible to do this acutely in some cases. Gradual attenuation, which results in the closure of the shunt over several weeks, potentially reduces the risk of portal hypertension and allows shorter surgical times. If complete attenuation is not achieved by the attenuation device following surgery, as assessed by follow up imaging, complete attenuation of the remaining shunting vessel is possible, by closing a preplaced suture loop (see figure 2) during a subsequent surgery. This however is rarely necessary.
Assessing improvement based upon an improvement in clinical signs alone can be very subjective, and usually a combination of an improvement in clinical signs, a documented lack of shunting on imaging, an increase in body weight and normalisation of biochemical parametres would be sought. George continues to do very well at home and his owners are happy they decided to pursue surgical management.
If you have a case you feel would benefit from further investigation or surgery then please contact SCVS, where one of the clinicians would be happy to discuss the case with you.